How likely is it that most of the general public will take a Covid-19 vaccine once one becomes available? Based on the first wave of survey data, the consensus is: likely. But are we asking the right questions? THREAD
Below I’ve put together some of the findings from studies that address the question of Covid-19 vaccine acceptance. If you would like more detail, I have put together this google doc with extra info on all the studies mentioned here and more that aren't https://docs.google.com/spreadsheets/d/1NWINNQBgdgClejuonre-nzulNqgI7MiJ9oixZNSV3Ck/edit?usp=sharing
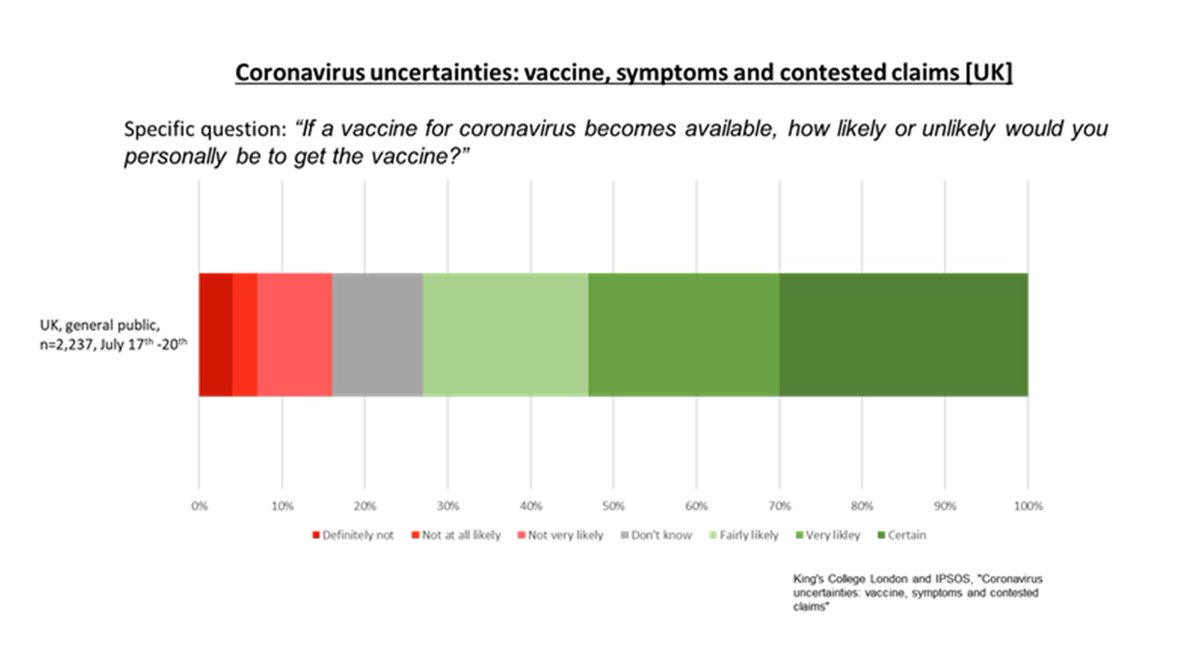
To try and find out if people are willing to take a Covid-19 vaccine when/if one finally becomes widely available, researchers have typically been asking the public questions that look somewhat like this:
This question is fine, but leave us little room to understand the really important group of people that fall within the “Don’t know” category. When a Covid-19 vaccine is available will these hesitant/undecided people likely end up accepting or rejecting the vaccine?
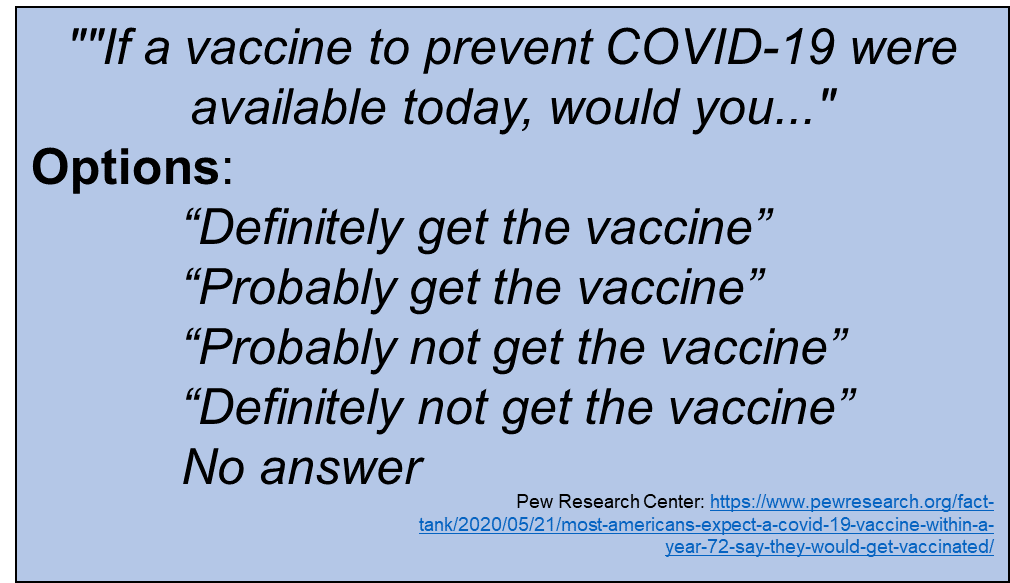
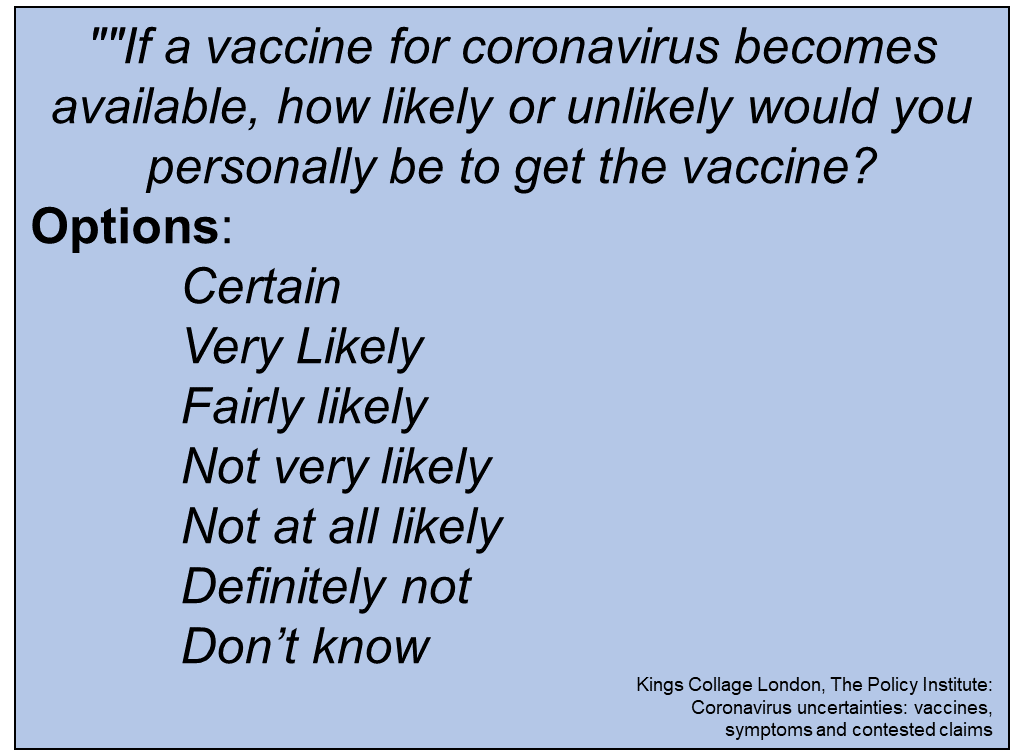
To get an indication of where the vaccine hesitant may land on this decision, we can just add more options to the question, like this:
Slight variations on these questions have now been asked in different countries and we're starting to build up an indication of a strong willingness to acceptance a Covid-19 vaccine. Here are a few stats, from those that have fully reported their findings on this question:
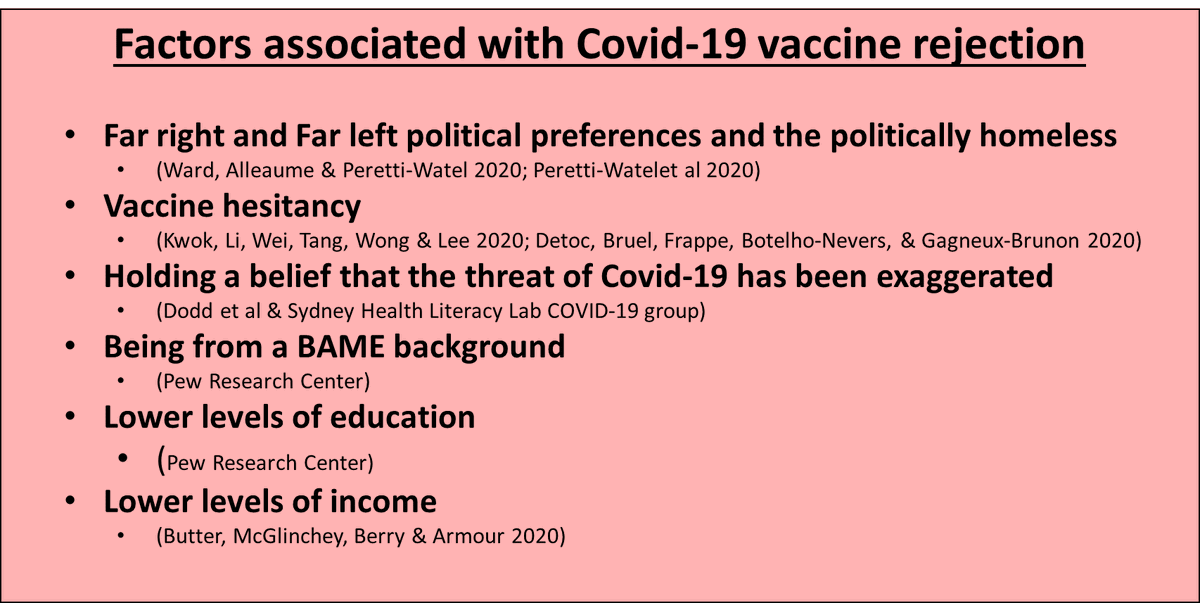
Across most of the Covid-19 vaccine acceptance studies, researcher have also conducted regression analysis to determine which factors are associated with an intended acceptance or rejection of the vaccine.
Across the studies I’ve seen so far, the following have been found to be associated with vaccine acceptance:
While all this research is great (and super interesting!) I can’t shake the feeling that we’ve skipped a step and not yet asked some important questions in regards to perception of the vaccine itself.
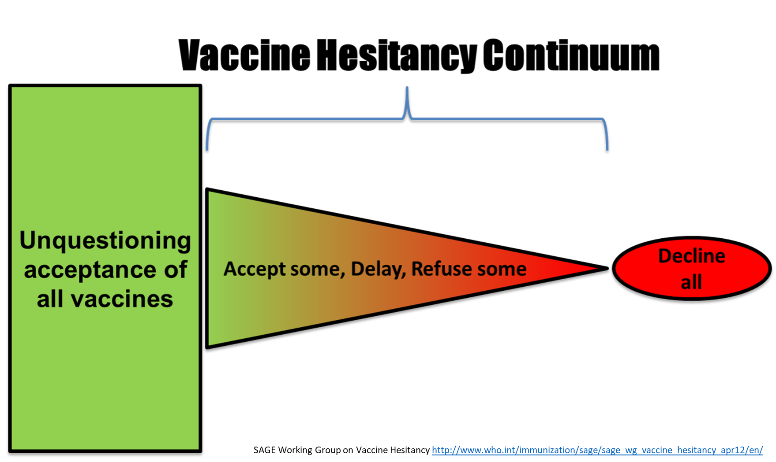
From previous research on vaccine hesitancy we know that not all vaccines are created equal in the eye of the (un)vaccinated. People are likely to be hesitant to different vaccines to different degrees.
Concerns about side-effects, concerns about vaccine effectiveness (efficacy) and different levels of availability all feed into the decision-making process.
For the Covid-19 vaccine, the importance of the vaccine’s efficacy on acceptance is demonstrated by the following study:
The study isn’t overly nuanced in its question, but with such a big difference here I’m concerned that not building possible vaccine characteristic into our research will likely lead to our questions being poor tool for predicting uptake.
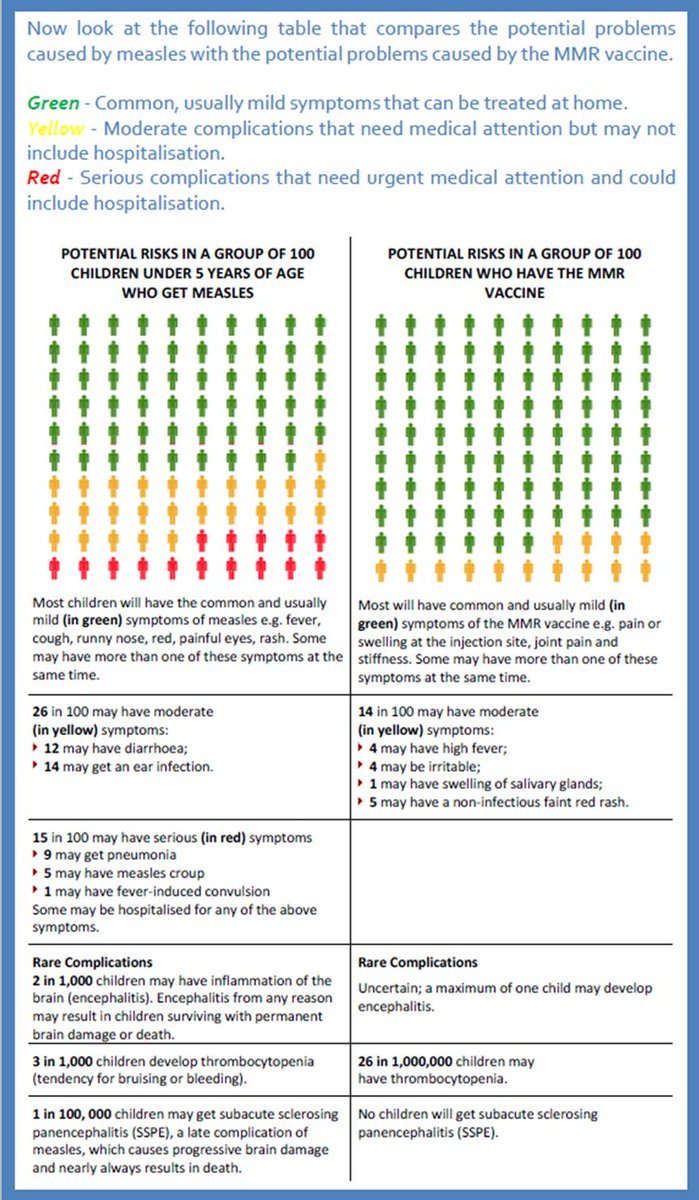
The same could be true of safety. What percentage of the public would accept a Covid-19 vaccine with similar side-effects to the meningitis vaccine? https://www.nhs.uk/conditions/vaccinations/men-b-vaccine-side-effects/ Who knows? But this is a question we could be investigating.
I’ve always liked the graphical representations of risks used in decision aids. Perhaps this could be worth investigating for Covid-19 and its different possible vaccines. http://www.ncirs.org.au/public/mmrv-vaccine-decision-aid
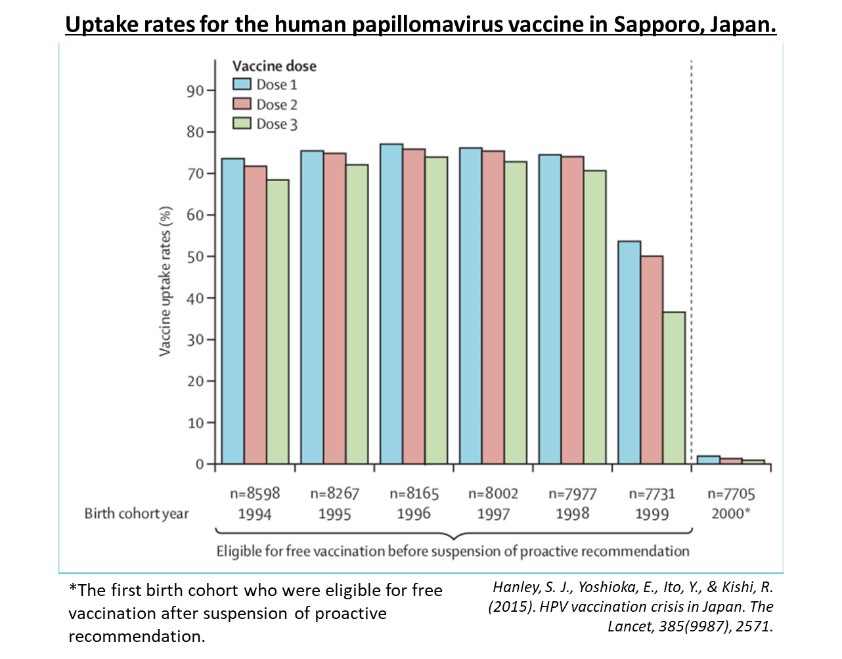
The issue of access, however, is the one that concerns me most. This is a graph of the HPV vaccination rate from Japan. In 2014, the country moved from proactively recommending to the vaccine being available on request. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)61152-7/fulltext
People could technically still ACCESS the vaccine but look at that change in uptake! A recommendation is therefore key, but who recommends the vaccine is also deeply important.
That leads us to the issue of trust, which I wont go into here but here’s one of my papers from my PhD that looks at that the complexities behind measuring trust in vaccination: https://www.tandfonline.com/doi/full/10.1080/21645515.2018.1459252
Further to the vaccine being recommended it will also need to be easily available. If we all have to set up an appointment through our GPs, expect a low uptake. If we get it at our local pharmacy maybe slightly better, if we can get it at our local community center even better.
That’s all I have for you today, myself, @SadieBellLSHTM , @DrPPaterson and Sandra Mounier-Jack from @LSHTM have two related papers that I will hopefully be able to share with you very soon.
Here’s the database again with all the paper I’ve mentioned in this thread: https://docs.google.com/spreadsheets/d/1NWINNQBgdgClejuonre-nzulNqgI7MiJ9oixZNSV3Ck/edit?usp=sharing Comments have been enabled so please let me know if I’ve missed any interesting papers on this topic and I’ll try to keep it updated.

 Read on Twitter
Read on Twitter