1/6 At yesterday's Emory IM COVID #JournalClub, I presented a great article ( @SHEA_Epi) on bacterial/fungal co-infection among COVID patients - from the Bronx at the height of the pandemic!
Here are some highlights
highlights  from the study by Nori et al. #MedTwitter #tweetorial
from the study by Nori et al. #MedTwitter #tweetorial
Here are some
 highlights
highlights  from the study by Nori et al. #MedTwitter #tweetorial
from the study by Nori et al. #MedTwitter #tweetorial
2/6 First, it looked at all #COVID patients Mar 1-Apr 18, which was ~ the pandemic zenith in NYC. (Visual aid from @COVID19Tracking via @TheAtlantic). Total (+) by PCR? 4,267.
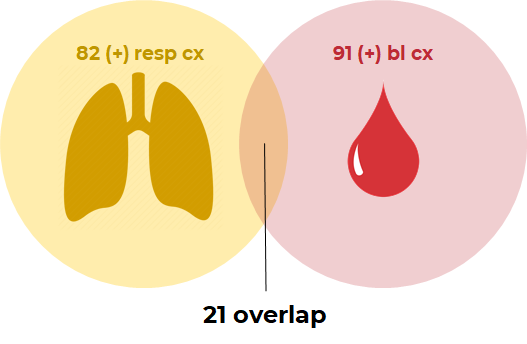
3/6 Then, they did a retrospective chart review. Total patients with (+) respiratory or bloodstream cultures? 152.
For those crunching the numbers, that's just 3.6%!
For those crunching the numbers, that's just 3.6%!
4/6 And that 3.6% was pretty sick:
 95%
95%  cultures = ICU
cultures = ICU
 54% of
54% of  cultures = CVCs, HD catheters, etc.
cultures = CVCs, HD catheters, etc.
 8 candidemia (7/8 = #CLABSI)
8 candidemia (7/8 = #CLABSI)
CRP & Procal were not helpful in distinguishing [COVID] from [COVID+co-infection]. Ex. IQR was 0-37 CRP, 0-10 procal.
IQR was 0-37 CRP, 0-10 procal.
 95%
95%  cultures = ICU
cultures = ICU 54% of
54% of  cultures = CVCs, HD catheters, etc.
cultures = CVCs, HD catheters, etc. 8 candidemia (7/8 = #CLABSI)
8 candidemia (7/8 = #CLABSI)CRP & Procal were not helpful in distinguishing [COVID] from [COVID+co-infection]. Ex.
 IQR was 0-37 CRP, 0-10 procal.
IQR was 0-37 CRP, 0-10 procal.
5/6 Most also seemed to develop those infections after arrival: median time-to-(+) 7d for  and 6d for
and 6d for  . A lot of co-infections were in immunocompromised (55%).
. A lot of co-infections were in immunocompromised (55%).
Yet 71% of ALL COVID(+) patients in the study got antibiotics. ? ? As the authors say, "a significant mismatch."
? As the authors say, "a significant mismatch."
 and 6d for
and 6d for  . A lot of co-infections were in immunocompromised (55%).
. A lot of co-infections were in immunocompromised (55%).Yet 71% of ALL COVID(+) patients in the study got antibiotics. ?
 ? As the authors say, "a significant mismatch."
? As the authors say, "a significant mismatch."
6/6 So what should we take away?
 Bacterial/fungal co-infection is rare (3.6%) in COVID
Bacterial/fungal co-infection is rare (3.6%) in COVID
 Look for it in the very sick (tubes/lines) who are already admitted
Look for it in the very sick (tubes/lines) who are already admitted
 Don't forget candida
Don't forget candida 
 Don't rely on CXR, CRP, or Procal
Don't rely on CXR, CRP, or Procal
 Be judicious with antibiotics!
Be judicious with antibiotics!
 Bacterial/fungal co-infection is rare (3.6%) in COVID
Bacterial/fungal co-infection is rare (3.6%) in COVID Look for it in the very sick (tubes/lines) who are already admitted
Look for it in the very sick (tubes/lines) who are already admitted Don't forget candida
Don't forget candida 
 Don't rely on CXR, CRP, or Procal
Don't rely on CXR, CRP, or Procal Be judicious with antibiotics!
Be judicious with antibiotics!

 Read on Twitter
Read on Twitter