New piece on subclinical TB in @ATSBlueEditor by the thoughtful @emilyakendall and @soustha - ahead-of-print paywall (working on it), so here's a quick thread, using figures presented elsewhere.
Many of these concepts are relevant to COVID-19 as well...
https://bit.ly/2IGPWMo
Many of these concepts are relevant to COVID-19 as well...
https://bit.ly/2IGPWMo
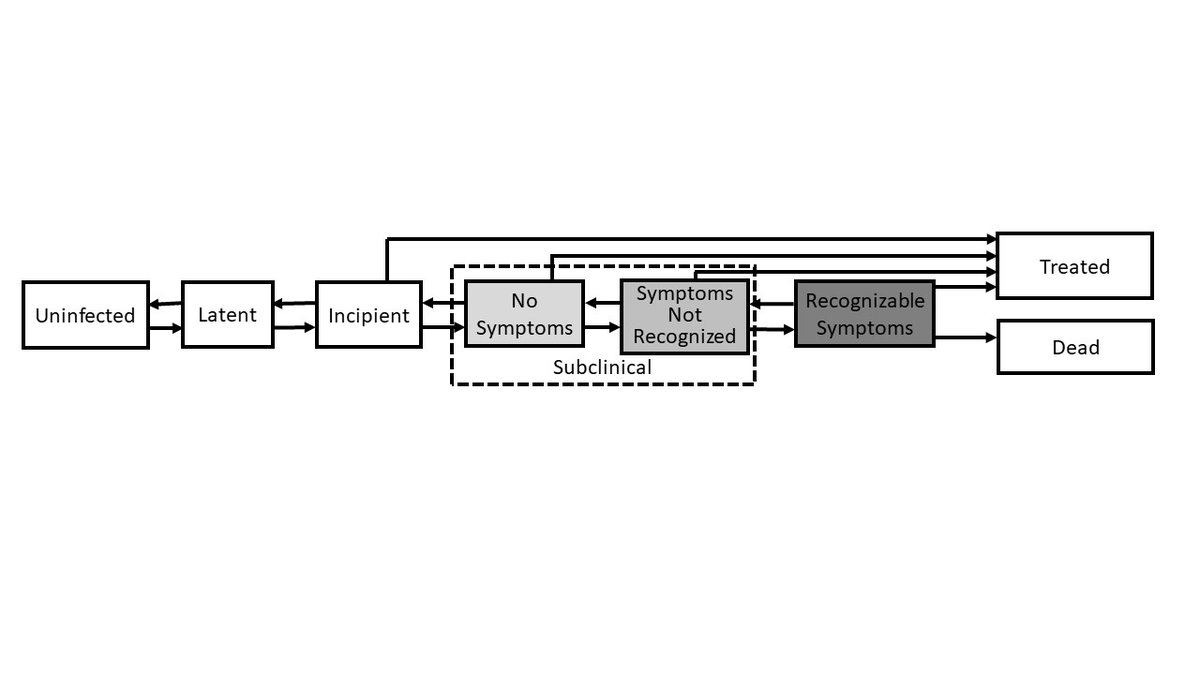
1. It's time to discard the binary concept of TB as "active" or "latent". We know that TB progresses thru incipient & subclinical phases - but subclinical disease can also regress, may cause sx's that aren't recognized, and can be diagnosed & treated (w/s shorter regimens?)
2. We can use prevalence survey data to infer burden of subclinical TB - great work recently on this also by @Rein_Houben & team. Likely at least 7 million people with prevalent subclinical TB, many of whom may have unrecognized symptoms + culturable sputum.
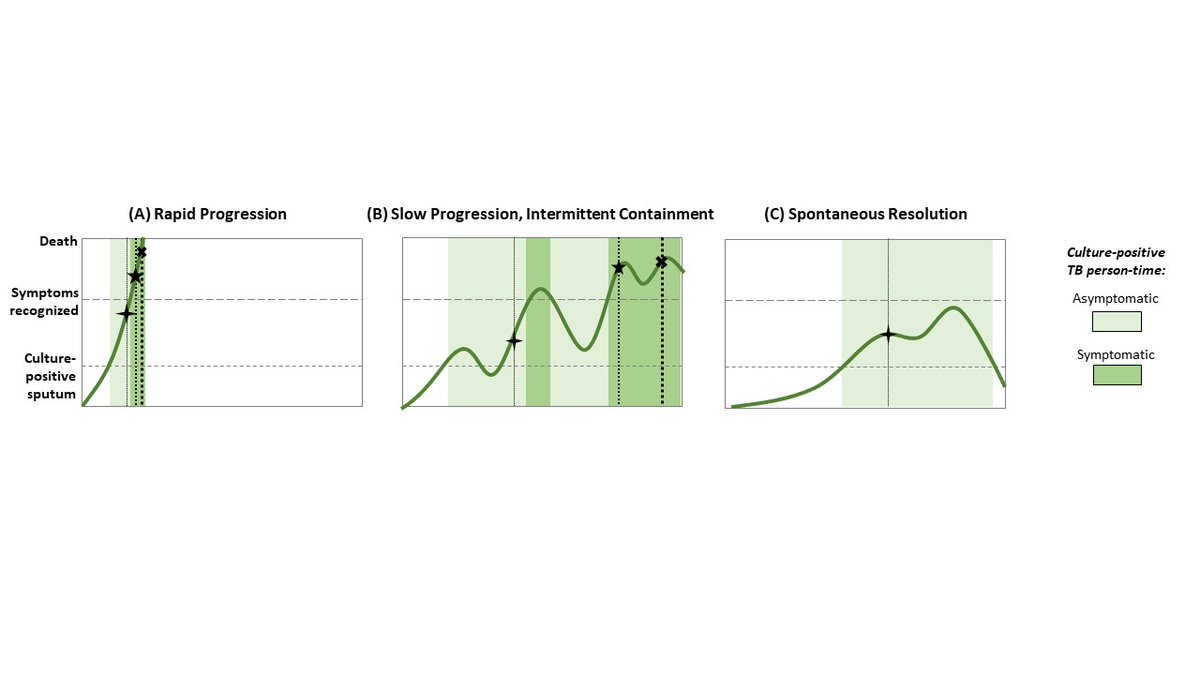
3. Clinical/natural history trajectories of people w/ subclinical TB likely to be very different - some will progress rapidly to severe disease, others will progress slowly, others will regress after long subclinical phase. The latter 2 likely more relevant to transmission...
Summary:
1. TB disease is a spectrum of infectiousness, symptoms, treatability, & diagnosability.
2. More than 50% of people with prevalent, culture-positive TB will respond "no" to symptom screen.
3. Trajectories of TB are heterogeneous - impt to learn when transmission occurs.
1. TB disease is a spectrum of infectiousness, symptoms, treatability, & diagnosability.
2. More than 50% of people with prevalent, culture-positive TB will respond "no" to symptom screen.
3. Trajectories of TB are heterogeneous - impt to learn when transmission occurs.

 Read on Twitter
Read on Twitter