STUDY: We offered antibody testing to >300 residents/staff at long-term care homes following large outbreaks. At a time when #COVID19 continues to be a major risk in homes, the findings validate aspects of our approach, support improvements, and when applied may save lives. 1/
At the top, I want to applaud medical resident @RVijh, who has worked closely with our team in LTC outbreaks and had a lead role in this study. (Not least of all as lead author of this paper!) As well, @CDCofBC was a crucial partner on this! https://www.ajicjournal.org/article/S0196-6553(20)30927-5/fulltext 2/
So, what did we do? In a nutshell (in two buildings, in fact), we offered serological testing to all residents/staff of two LTC homes where large COVID-19 outbreaks had taken place. These OBs were in March-April; among our first, and we were learning every day. (We still are.) 3/
303 people generously participated, each providing a blood sample which was tested for antibodies to SARS-CoV-2 (evidence of past infxn). With 12 samples excluded due to indeterminate results, we determined infection history (or lack thereof) for 122 residents and 169 staff. 4/
For 113 of these 291 people, bloodwork showed a history of previous infection (“reactive serology”: antibodies to the SARS-CoV-2 virus detected). Among these previously infected residents and staff, 16% HAD NO HISTORY OF SYMPTOMS BEING NOTED (15% of residents, 18% of staff). 5/
Also among the 113 residents and staff with previous infection shown by serology, 29% HAD NO HISTORY OF A POSITIVE TEST (26% of residents, 33% of staff). They had not been tested, or they had negative tests recorded… 6/
…I can’t stress this enough: this study came after large outbreaks, in which staff/residents were closely monitored, and tested if showing symptoms. Entire floors were screened at times (w/o symptoms). Yet, with retrospective serology, we found that infections can be missed. 7/
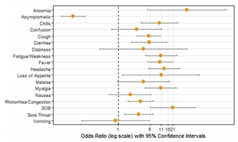
And ‘hidden infections’ weren’t the only story here. An important 15% of those with antibodies detected had no history of symptoms, but the majority did. Important: nonspecific symptoms (fatigue, aches...) were as strongly associated as with infxn history as cough/fever. 8/
For people working to address COVID-19 outbreaks in long-term care, what can we do with this information? We think the implications are clear... 10/
1. Continue a “test on sight” approach to any symptoms/changes in resident status. Empower staff, who know the residents, to take a low-barrier approach. I like to say to Directors of Care: ‘If a nurse asks to test a resident, the swab can automatically be taken. They know.’ 11/
(When it comes to COVID-19 testing, the friction should be in the nasopharynx, not the processes to request and take a swab.) 12/
2. SUPPORT long-term care workers to access testing and stay home when experiencing ANY symptoms. Homes that provide paid sick leave naturally have less risk of staff working with low-grade symptoms to maintain a livelihood. (A higher wage wage to start with would also help.) 13/
3. If you haven’t already, redefine ‘symptoms.’ To make (1) and (2) most effective, in the context of LTC (high risk setting) and particularly during an outbreak (high pretest probability) the care team needs to be vigilant for even minor symptoms in residents AND staff. 14/
We still manage outbreaks in which many cases are identified in early days; spread has occurred before the first case is diagnosed. This iceberg phenomenon suggests that we need to look very closely for new cases, so as to identify/stop transmission sooner rather than later. 15/
Please share in your LTC/public health communities! I am unabashed in trying to push this out. With high rates of COVID-19 in the community, LTC workers and in turn the residents they care for are at risk. Outbreaks with dozens of residents infected still occur, and… 16/
…Observed case fatality rates among LTC residents mean that 1 in 3 cases are likely to pass away. *Or, as I like to think of it, if we prevent 30 cases we might save 10 lives in a single care home.* There is so much to gain when we get this right. Thanks for reading! 17/17

 Read on Twitter
Read on Twitter