We recently published the 4th results paper from @SNAPs_News SNAP-2: EPICCS in @Anaes_Journal #openaccess
…https://associationofanaesthetists-publications.onlinelibrary.wiley.com/doi/full/10.1111/anae.15302
We ran a survey alongside our main observational cohort study, and looked at the perceptions of clinicians about postoperative critical care. 1/n
…https://associationofanaesthetists-publications.onlinelibrary.wiley.com/doi/full/10.1111/anae.15302
We ran a survey alongside our main observational cohort study, and looked at the perceptions of clinicians about postoperative critical care. 1/n
We received 10,383 survey responses from 237 hospitals across the UK, and used both qualitative and quantitative methods to analyse these responses. 2/n
We found that consultants were significantly more likely to refer patients of lower‐risk than recommended by national guidelines to postop critical care (≤ 5% 30‐day mort risk; 27.7% of consultants vs. 18.2% of non‐consultants, chi‐squared statistic = 44.4287, p < 0.0001). 3/n
The majority of respondents reported that critical care provision was inadequate, and cited the value of critical care as being predominantly due to higher nurse: patient ratios. 4/n
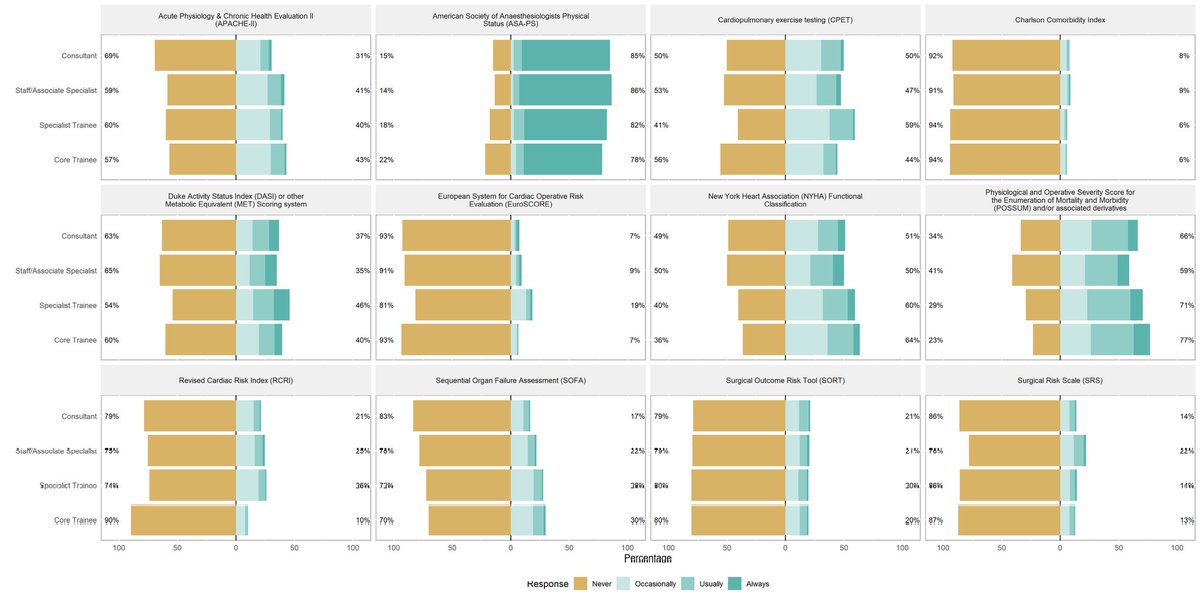
The ASA physical status scale was the most widely reported risk stratification tool reportedly used by participants select ‘always used’. 5/n
Five core themes were found in the qualitative analysis of free‐text responses to the question of whether respondents felt there was enough critical care capacity at their institution: lack of capacity; variability; cancellations; hospital beds; and service‐wide factors. 6/n
Respondents generally thought critical care was beneficial due to higher levels of observation and quicker interventions. Themes derived were advantages, staff, timings, patients, evidence and limitations. 7/n
The perceived advantages of critical care over ward‐based care illustrated that participants thought critical care could avoid poorer outcomes, with improved capacity for monitoring and management. 8/n
Staffing was another key theme, with participants stating a higher nurse to patient ratio in critical care, leading to better outcomes. This was further supported by comments on ward‐based care being frequently understaffed. 9/n
There are lots more to unpick from this paper than Tweets would ever do justice. Please check out the paper. Many thanks to all @SNAPs_News collaborators, @HSRCNews, @sourceuclh for helping facilitate the study. And to @rmoonesinghe and @drstevok for supervising. 10/n
Thanks also to @Assoc_Anaes and @NIAAResearch, @UCLHresearch, @NIHRresearch, and @RCoANews for funding and other support for the study. 11/n
Most of all, thanks to Sophia Hashim, our EXCELLENT med student (now FY1 at St Mary's Hospital). She did the bulk of analysis and led the manuscript writing. She started analysis as a 4th year med student and saw it through to publication under difficult COVID19 conditions. 12/12

 Read on Twitter
Read on Twitter