Hope better late than never true here @DrAbdulRazak_MD. Twitter sat in the back seat during the holidays & in the trunk while on clinical service...
Enjoyed the read. Compelling rationale, well reported, thoughtful discussion. Useful data despite undesired outcome.
#neoebm 1/? https://twitter.com/nbamat/status/1341047278493167618
Enjoyed the read. Compelling rationale, well reported, thoughtful discussion. Useful data despite undesired outcome.
#neoebm 1/? https://twitter.com/nbamat/status/1341047278493167618
Regarding right-shift model as an outcome...
Why compelling? For me, key reason is it provides an objective measure of impaired gas exchange. An ongoing limitation of BPD definitions is that classifications based on therapy provided - an imperfect surrogate of underlying dz.
2/
Why compelling? For me, key reason is it provides an objective measure of impaired gas exchange. An ongoing limitation of BPD definitions is that classifications based on therapy provided - an imperfect surrogate of underlying dz.
2/
Second, it's somewhat practical. Can be done at cotside w/o blood draws or expensive equipment. You essentially need a pulse-ox and a variable source of FiO2.
3/
3/
Also agree w/ @jane_pillow on the convenience of continuous outcomes. Helps minimize statistical information loss and reduce the sample size. But, those pragmatic bits are limited w/o knowing if (& how much) right-shift is a/w clinically meaningful long-term outcomes.
4/
4/
Why limited? 2 key reasons: (1) outcome prone to measurement error (2) value influenced by underlying respiratory support.
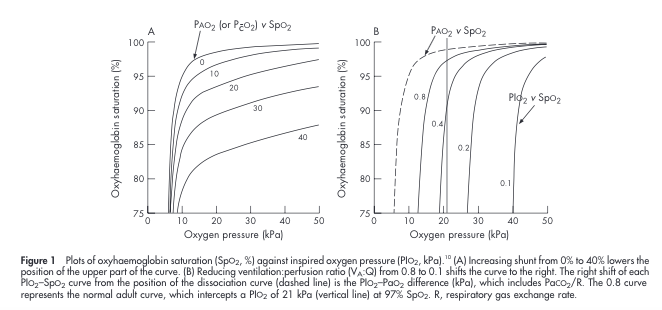
To elaborate, helpful to review how right-shift derived.
Fig is from 2006 paper by @Boyleem @StensonBen & others in @ADC_FN: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2672753/pdf/F409.pdf
5/
To elaborate, helpful to review how right-shift derived.
Fig is from 2006 paper by @Boyleem @StensonBen & others in @ADC_FN: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2672753/pdf/F409.pdf
5/
To obtain right-shift, the investigator inputs a series of FiO2/SpO2 pairs & the model superimposes a curvilinear best-fit over the data. On the basis of the position & shape of the resulting curve (relative to an ideal), the model estimates BOTH right-shift and shunt.
6/
6/
I think of right-shift as impaired gas exchange from things that are RESPONSIVE to FiO2 - V/Q mismatch, hypoventilation, diffusion, low PiO2 (altitude). In contrast, intra and extrapulmonary shunt have little response to increased FiO2
7/
7/
So getting back to the first limitation; (1) outcome prone to measurement error. The estimates of right-shift and shunt are only as good as the FiO2/SpO2 data you input. Neonatal providers know how inexact SpO2 measures can be, and..
8/
8/
the curvilinear nature of the model complicates; if u don't obtain SpO2/FiO2 pairs above & below the "knee" of the curve, estimation of right-shift & shunt are unstable. This can be a challenge; i.e. an infant w/ high SpO2 @ 21%. A strength of the study was use of FiO2 <21%
9/
9/
The second limitation is that a right-shift value is directly influenced by underlying respiratory support. For example, If I took a babe w/ high FiO2 & low SpO2 values (high right-shift) b/c of atelectasis on 1/4 L NC & started nCPAP the SpO2 for a given FiO2 would improve
10/
10/
So it's hard to make sense of right-shift values across subjects on different degrees of respiratory support. Apples to oranges. IMO, you should adjust for type and degree of respiratory support in some way.
11/
11/
In sum, it's a compelling, convenient outcome measure that I'm happy to see getting more exposure, but it's imperfect, nuanced, and needs further study.
Hope this was helpful!
12/12
Hope this was helpful!
12/12

 Read on Twitter
Read on Twitter